Seeking
innovation
for
evaluations?

U.S. Patent 10,646,136
An Original Tool for the Clinic: The Heel Height Knee Square
Kevin G. Cummings, PT, DPT, MSA
Disclosure: The studies mentioned below are listed as concepts and application examples. The research articles’ authors below have no financial relationships with HHEEL Height Knee Square, LLC.
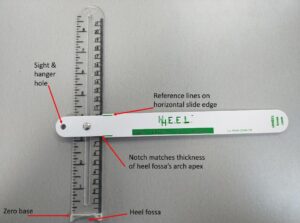
Engineered in Burlington, VT, the Heel Height Knee Square™ accurately assesses 8 extension and 6 flexion perspectives, plus 3 foot and ankle applications.
University of Vermont Department of Orthopedics reiterates the functional importance to address extension after ACL reconstruction.[1] A measuring method was validated by the Steadman Hawkins Clinic: 1 cm change in heel-height difference corresponded to a 1.2° alteration in knee extension. The Vail researchers’ conclusion: “this test is more meaningful and easier for detecting subtle knee flexion contractures.”[2] Another article at the same institute noted “…side to side difference of 3 cm in the heel height test was both highly sensitive and specific for the detection of concominant ACL-FCL injury…”[3]
Now, there is a versatile T-square ruler available to ascertain such markers.
Analyzing the contralateral versus the injured knee is important, especially when there is loss of motion.[4] Wilk et al. report, “hyperextension is imperative to a successful outcome” after ACL reconstruction, and they compare to the uninjured knee.[5] Shelbourne et al. state, “a difference in extension kinesthetically, is to passively extend the patient’s knee by holding the thigh in place with one hand and using the other hand to hold the ball of the foot to lift the heel off the examination table.”[6] Other authors noted with extension lift, “a heel height > 5 cm was an independent predictor for ACL failure.”[7] Heel lift during the Lever test has been critically analyzed.[8] Genu recurvatum can be a risk factor for ACL injury.[9] Regaining terminal knee active extension can be challenging; often patients have an extension lag, which has been defined as greater than 5 degrees from full extension.[10]
In cases of knee arthrofibrosis, 90° is considered a goal to achieve.[11] Knee flexion tested in prone is a reliable indicator for quadriceps flexibility.[12] Whereas, full knee flexion ROM symmetry equates to a patient’s kneeling ability by sitting back on the heels.[13] Furthermore, a basic heel slide is one method to assess knee flexion.[14] The amount of posterior translation, in a PCL deficient knee, has been studied.[15]
Physical therapists determined the Lunge Test had more reliability than standard goniometer for measuring ankle dorsiflexion.[16] This has relevance since limited dorsiflexion may be an ACL injury risk factor.[17] Also, athletic trainers have documented an association between navicular drop and anterior knee laxity.[9],[18],[19] Finally, a heel-rise test and height screening provide outcome measures for Achilles tendon rehabilitation.[20]
It has been aptly said by Terry Malone, “If you don’t measure something, you don’t know it.”[21] A need in the clinic has been met: These aforementioned measurements plus others can be quantified with the unique Heel Height Knee Square™.
Footnotes
[1] Beynnon, B. D., Johnson, R. J., Abate, J. A., Fleming, B. C., & Nichols, C. E. (2005). Treatment of anterior cruciate ligament injuries, part I. The American journal of sports medicine, 33(10), 1579-1602.
[2] Schlegel, T. F., Boublik, M., Hawkins, R. J., & Steadman, J. R. (2002). Reliability of heel-height measurement for documenting knee extension deficits. The American journal of sports medicine, 30(4), 479-482.
[3] Cinque, M. E., Geeslin, A. G., Chahla, J., Moatshe, G., Pogorzelski, J., DePhillipo, N. N., & LaPrade, R. F. (2017). The heel height test: a novel tool for the detection of combined anterior cruciate ligament and fibular collateral ligament tears. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 33(12), 2177-2181.
[4] Harner, C. D., Irrgang, J. J., Paul, J., Dearwater, S., & Fu, F. H. (1992). Loss of motion after anterior cruciate ligament reconstruction. The American journal of sports medicine, 20(5), 499-506.
[5] Wilk, K. E., Macrina, L. C., Cain, E. L., Dugas, J. R., & Andrews, J. R. (2012). Recent advances in the rehabilitation of anterior cruciate ligament injuries. journal of orthopaedic & sports physical therapy, 42(3), 153-171.
[6] Shelbourne, K. D., Urch, S. E., Gray, T., & Freeman, H. (2012). Loss of normal knee motion after anterior cruciate ligament reconstruction is associated with radiographic arthritic changes after surgery. The American journal of sports medicine, 40(1), 108-113.
[7] Larson, C. M., Bedi, A., Dietrich, M. E., Swaringen, J. C., Wulf, C. A., Rowley, D. M., & Giveans, M. R. (2017). Generalized hypermobility, knee hyperextension, and outcomes after anterior cruciate ligament reconstruction: prospective, case-control study with mean 6 years follow-up. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 33(10), 1852-1858.
[8] Massey, P. A., Harris, J. D., Winston, L. A., Lintner, D. M., Delgado, D. A., & McCulloch, P. C. (2017). Critical analysis of the lever test for diagnosis of anterior cruciate ligament insufficiency. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 33(8), 1560-1566.
[9] Vacek, P. M., Slauterbeck, J. R., Tourville, T. W., Sturnick, D. R., Holterman, L. A., Smith, H. C., … & Beynnon, B. D. (2016). Multivariate analysis of the risk factors for first-time noncontact ACL injury in high school and college athletes: a prospective cohort study with a nested, matched case-control analysis. The American journal of sports medicine, 44(6), 1492-1501.
[10] Carlson Strother, C. R., LaPrade, M. D., Keyt, L. K., Wilbur, R. R., Krych, A. J., & Stuart, M. J. (2021). A strategy for repair, augmentation, and reconstruction of knee extensor mechanism disruption: a retrospective review. Orthopaedic Journal of Sports Medicine, 9(10).
[11] Millett, P. J., Williams, R. J., & Wickiewicz, T. L. (1999). Open debridement and soft tissue release as a salvage procedure for the severely arthrofibrotic knee. The American Journal of Sports Medicine, 27(5), 552-561.
[12] Piva, S. R., Goodnite, E. A., & Childs, J. D. (2005). Strength around the hip and flexibility of soft tissues in individuals with and without patellofemoral pain syndrome. Journal of orthopaedic & sports physical therapy, 35(12), 793-801.
[13] Shelbourne, K. D., & Klotz, C. (2006). What I have learned about the ACL: utilizing a progressive rehabilitation scheme to achieve total knee symmetry after anterior cruciate ligament reconstruction. Journal of Orthopaedic Science, 11(3), 318-325.
[14] Haro, M. S., & Shelbourne, K. D. (2016). Prevention and management of loss of motion in anterior cruciate ligament surgery. Operative Techniques in Sports Medicine, 24(1), 45-54.
[15] Hewett, T. E., Noyes, F. R., & Lee, M. D. (1997). Diagnosis of complete and partial posterior cruciate ligament ruptures: stress radiography compared with KT-1000 arthrometer and posterior drawer testing. The American journal of sports medicine, 25(5), 648-655.
[16] Konor, M. M., Morton, S., Eckerson, J. M., & Grindstaff, T. L. (2012). Reliability of three measures of ankle dorsiflexion range of motion. International journal of sports physical therapy, 7(3), 279.
[17] Wahlstedt, C., & Rasmussen-Barr, E. (2015). Anterior cruciate ligament injury and ankle dorsiflexion. Knee Surgery, Sports Traumatology, Arthroscopy, 23(11), 3202-3207.
[18] Shultz, Sandra J., William N. Dudley, and Yanfang Kong. “Identifying multiplanar knee laxity profiles and associated physical characteristics.” Journal of athletic training 47.2 (2012): 159-169.
[19] Allen, Mary K., and Ward M. Glasoe. “Metrecom measurement of navicular drop in subjects with anterior cruciate ligament injury.” Journal of athletic training 35.4 (2000): 403.
[20] Silbernagel, Karin Grävare, Robert Steele, and Kurt Manal. “Deficits in heel-rise height and Achilles tendon elongation occur in patients recovering from an Achilles tendon rupture.” The American journal of sports medicine 40.7 (2012): 1564-1571.
[21] Terry Malone, PT, EdD, ATC, FAPTA online seminar. “What Every Clinician Should Know About ACL Injury and Treatment.” MedBridge.
